The 3 Wishes Project
End-of-life care in the ICU is a difficult experience for all involved. Families are struggling with the impending death of their loved one. The altered level of consciousness for many critically ill patients means loss of their autonomy and personhood. It may be particularly difficult for grieving families to spend the last hours and days together with the patient surrounded by technology. Working in this environment also takes a toll on clinicians. Being surrounded by grief can be emotionally and psychologically difficult. Thus, dying in the complex, efficiency-driven environment of the ICU can be dehumanizing for the patient, and have profound, long-lasting consequences for all persons attendant to that death.
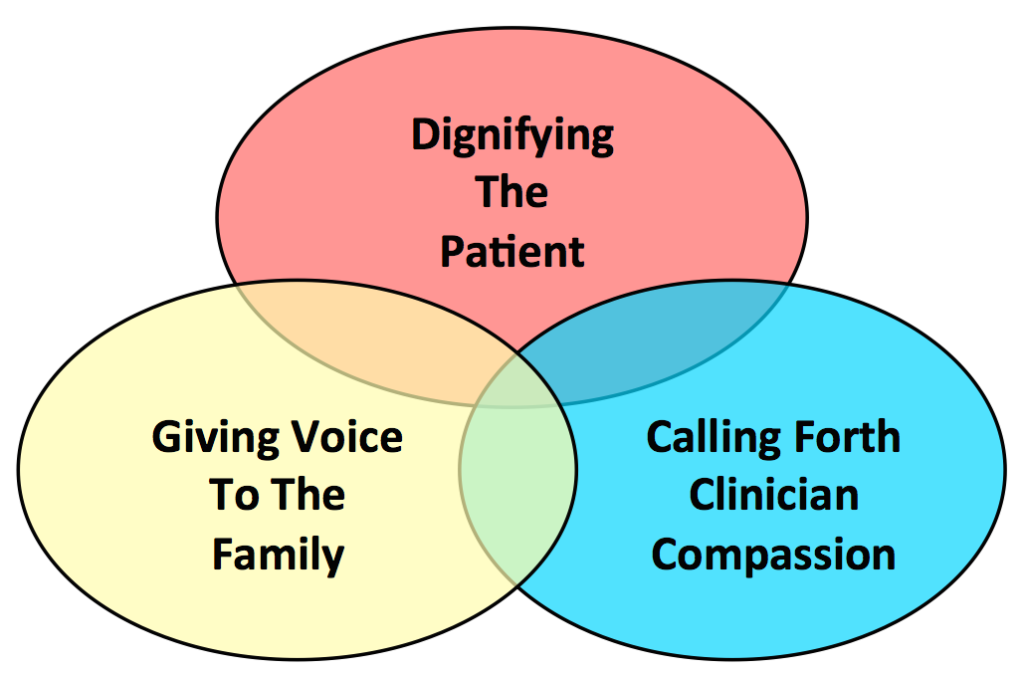
With these challenges in mind, we developed the 3 Wishes Project. The aim is to recognize the inherent dignity of the dying patient, and forge connections among patients, family members and clinicians to try to ease the grieving process. The original objectives of the 3 Wishes Demonstration Project were: 1) for patients, to honour their inherent dignity and celebrate their legacy; 2) for family members, to humanize the dying experience and create positive memories; and 3) for clinicians, to foster patient-and family-centered care and inspire a deeper sense of vocation. This is achieved by eliciting and implementing wishes that are meaningful at the end of life. Wishes are typically simple and inexpensive, yet experienced positively - a taste of food or beverage under the tongue, a visit by the family pet, favourite music playing in the room, a final toast, or surrounding the patient by things and people that they love.
The first 3 Wishes Demonstration Project was conducted in a 21-bed medical-surgical ICU in a tertiary care hospital, St. Joseph's Healthcare in Hamilton, 1 week per month from January 2013 - November 2014. Patients and families were invited to participate when they had made the decision to withdraw advanced life support in anticipation of death, or if the probability of patient dying in the ICU was >95% as judged by the physician. By eliciting, then implementing a set of 3 wishes identified by patients, families, clinicians or the 3 Wishes Project team, our focus was personalizing end of life care.
What did we find? For the patient, eliciting then implementing the 3 wishes encouraged individualized end-of-life care, guiding us to see the dying patient as a person. For the family, the 3 Wishes Project helped to create enduring positive memories to carry forth, countering the negative visual, auditory and tactile stimuli propagated by technology. For clinicians, it promoted inter-professional care, strengthened team bonds and exemplified humanism in practice. For clinicians-in-training, the 3 Wishes Project offered experiential, case-based, palliative care education.
The wishes are mostly a heuristic - and they also represent acts of compassion. They're a way to start a conversation about who the patient is as a person, and what matters most at the end of their life. In the ICU, many critically ill patients are unable to express themselves. Asking what the patient would wish for is an opportunity for family members and clinicians to connect on a human level. Implementing wishes provides families with something meaningful to do when the goals of care have shifted from curative to palliative care. The story-telling fostered by the 3 Wishes Project helps to reflect on patient preferences, journeys and legacies, underscoring our shared humanity. Implementing wishes provides clinicians with an opportunity to demonstrate their concern and respect for the patient and family in a tangible way. By integrating palliative care and spiritual care into critical care practice, the 3 Wishes Project also encourages the verbalization and realization of unmet spiritual needs, whether secular or faith-based.
In summary, the 3 Wishes Project underscores the drive that we all have to search for meaning, memories and closure in anticipation of death, while helping to create preparedness, comfort and connections during the dying process.